INTRODUCTION
Skin is the outermost covering and the largest organ of the integumentary system of our body. It protects deeper tissue from harsh environment, regulate temperature, and prevents loss of water; the sensory receptors attached to it are involved in detecting pain, pressure and temperature. other functions are insulation, vitamin D synthesis and immunity to protect against pathogen invaders, hence skin function as overall protection barrier but burns destroy the protection barrier but burns destroy the protection shield, and our body gets exposed to various external impetuses.
A burn occurs when heat, chemicals, sunlight, electricity or radiation damages skin tissue. Most burns happen accidentally. There are different degrees of burns. Your healthcare provider determines the seriousness (degree) of a burn based on the depth of the burn and the amount of affected skin. Burns can be painful. Left untreated, a burn can lead to infection.
Burn is associated with severe skin damage. therefore, serious burns injury needs immediate medical support to prevent further complication and death. Burns occurs when energy from a heat source is transferred to the tissues of the body. Heat may be transferred through conduction or electromagnetic radiation.
Burns
A burn is an injury to the skin or other organic tissue primarily caused by heat or due to radiation, radioactivity, electricity, friction or contact with chemicals.
Thermal (heat) burns occur when some or all of the cells in the skin or other tissues are
destroyed by :
- -hot liquids (scalds)-hot solids (contact burns)-flames (flame burns)
TYPES OF BURNS INJURY :
Primary Injury
It is the immediately damage caused by the burns . Little can be done to limit the primary injury in most cases of trauma. However a prompt removal of the heat source and rapid cooling of the burns limit the extent of primary injury
Secondary injury
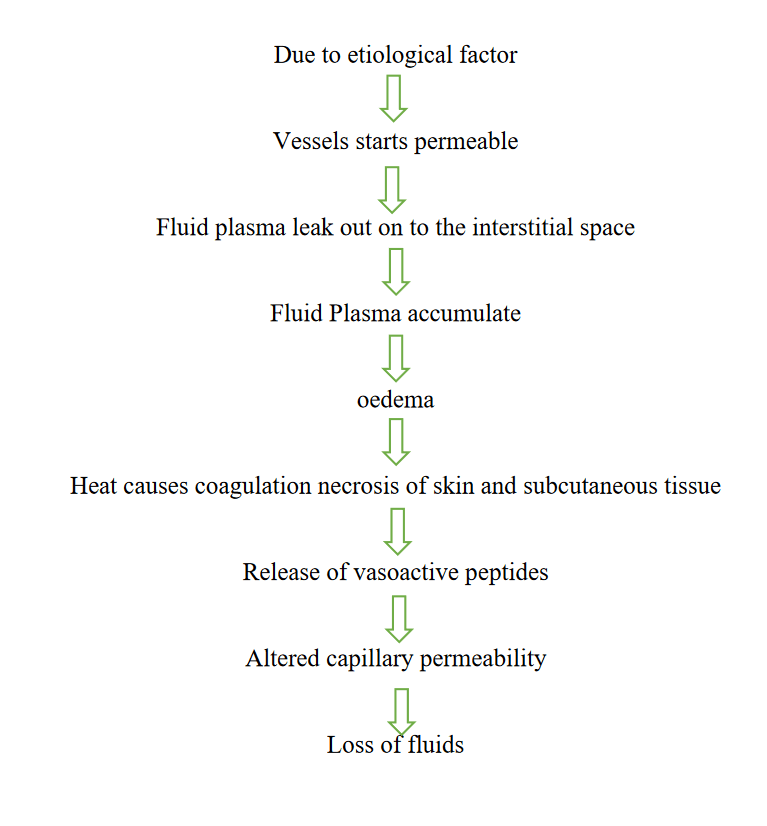
It is the deleterious effect resulting from the primary injury. A major burns can result in loss of fluids, secondary infection, endogenous and exogenous release of toxins, fluids shift , coagulopathy oedema , constriction caused by burns eschar.
CAUSES OF BURNS :
- -Thermal burns-Chemical burns-Electric burns-Radiation burns-Inhalation injury
CLASSIFICATION OF BURNS
A: According to burn depth :
• Superficial Partial thickness or 1st degree burns:
In this involve only upper layer of skin the epidermis ( skin surface).it usually produce a pink to reddish colour on the burned skin and very sensitive to touch and skin appear blanched when light pressure is applied. This burns is produce redness pain and minor swelling. Healing time is about 3 – 6 days.
• Deep partial thickness and second degree burns:
It affect both the outer layer ( epidermis ) and under layer lining of skin ( dermis ) causing redness, pain , swelling and blisters. There symptoms include red, blistered, and may be swollen and painful.
• Full thickness and third-degree burns:
Third-degree burns destroy the epidermis and dermis. They may go into the innermost layer of skin, the subcutaneous tissue. The burn site may look white or blackened and charred.
• Fourth-degree burns:
Fourth-degree burns go through both layers of the skin and underlying tissue as well as deeper tissue, possibly involving muscle and bone. There is no feeling in the area since the nerve endings are destroyed.
B) According to burn severity:
1) Minor Burns :
All 1st degree burns as well as second degree burns that involves less than 10% of the body surface usually are classified as minor
2) Moderate burns:
Burns involving hand s and feet face or genital , second degree burns involving more than 10 % body surface area . superficial partial thickness burns of the head hand and feet or perineum suspected child abuse concomitant trauma and significant pre-existing disease
3) Severe Burns :
Burns surface involvement of 25% body surface area .All third degree burns classified as moderate or more often or severe Full thickness burn 10% Body surface area.
C) According to the extent of body surface area injured:
Burns surface involvement of 25% body surface area .All third degree burns classified as moderate or more often or severe Full thickness burn 10% Body surface area.
✓ The rule of nine :
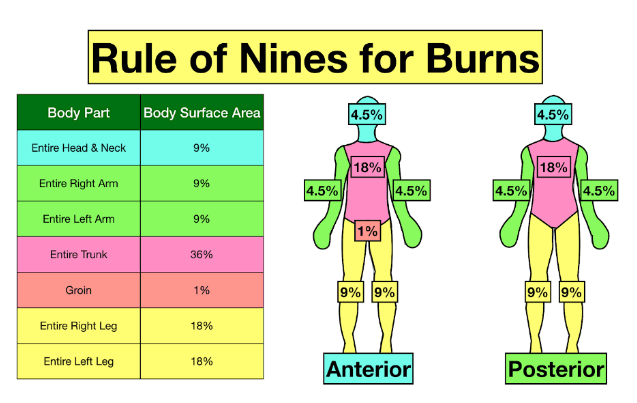
This allows the emergency medical provider to obtain a quick estimate of how much body surface area is burned. For example, if a patient's entire back (18%) and entire left leg (18%) are burned, about 36% of the patient's BSA is affected. The BSAs assigned to each body part refer to the entire body part. So, for example, if half of a patient's left leg were burned, it would be assigned a BSA value of 9% (half the total surface area of the leg). Thus, if a patient's entire back (18%), but only half of their left leg (9%) was burned, the amount of BSA affected would be 27%.
✓ Lund and Browder method :
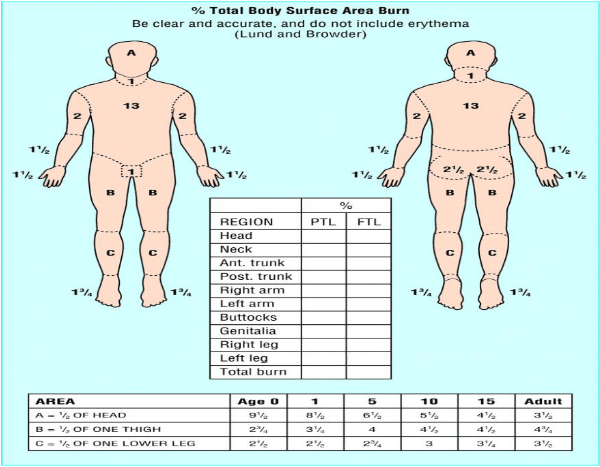
For children and infants, the Lund-Browder chart is used to assess the burned body surface area. Different percentages are used because the ratio of the combined surface area of the head and neck to the surface area of the limbs is typically larger in children than that of an adult.
✓ Palm method
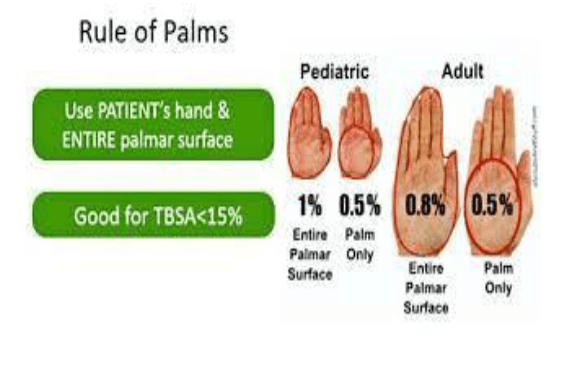
The "rule of palm" is another way to estimate the size of a burn. The palm of the person who is burned (not fingers or wrist area) is about 1% of the body. Use the person's palm to measure the body surface area burned. It can be hard to estimate the size of a burn
❖ Pathophysiology of burns :
❖ Diagnostic studies in burns:
1) Complete blood test : initial increased haematocrit (Hct) due to fluid loss, decreased haematocrits Hct and RBC may occur due to heat damage due to vascular endothelium.
2) ABG :
3) Serum electrolyte : hyponatremia fluid loss , potassium level may initially increased injured tissue.
4) Serum albumin : loss protein in fluid
5) Urine routine
6) Chest Xray
7) ECG
8) Bronchoscopy
Management of burns :
Burn managements can be organized chronologically into three phases emergent (resuscitative) , acute ( wound healing ) , and rehabilitative (restorative ) . For example , the emergent phase begin at the time of the burn injury, and care often begin in the prehospital phase, depending on the skill level of providers at the scene . Planning for rehabilitation begins on the day of the burn injury or admission to the burn center. Formal rehabilitation begins as soon as functional assessment can be performed . wound care is the primary focus on acute phase , but wound care also takes place in both the emergent and rehabilitation phase.
PREHOSPITAL PHASE :
• At the scene of the injury, priority is given to removing the person from the source of the burn and stopping the urning process.
• Small thermal burns ( 10 % or less of TBSA ) should be covered with a clean , cool, tap water dampened towel for the patients comfort and protection until medical care is available.
• If the burn is large ( greater than 10% TBSA ) or an electrical or inhalation burn is suspected , first focus ABC:
1) Airway management :
➢ Airway stability should be assessed rapidly in burns involving facial or suspected inhalation injuries, particularly in the early period following injury when the airway is at risk of obstruction due to swelling of the oropharynx and soft tissues of the neck.
➢ Airway burns, smoke inhalation syndrome, severe burns of face and neck, laryngeal edema may need intubation and tracheostomy.
2) Breathing :
Check adequacy of ventilation
3) Circulation :
- Check for the presence and regularity of pulses and elevate the burned limb above the heart to decrease pain and swelling
Hyperbaric oxygen therapy :
➢ Oxygen administration is pivotal increasing the gradient for oxygen binding to haemoglobin, so that unbound CO can be exhaled through the lungs. Oxygen saturation is an unreliable oxygenation parameter in 'patients with carbon monoxide poisoning.
➢ The use of HBOT, or hyperbaric oxygen, greatly reduces the burn victims chances of severe infection or death.
NURSING ASSESSMENT:-
➢ Remove jewellery and clothing in contact with burn source
➢ Cool affected area as soon as possible (within 3 hours from time of burn) for 20 minutes with cool running water
▪ If unavailable, other options include: frequently changed cold water compresses, immersion in a basin, irrigation via an open giving set
▪ Flush the affected area with copious amount of water to irrigate the skin anywhere from 20 min to 2 hour postexposure 15
➢ Never apply ice and avoid use of hydrogel burn products, since this can cause hypothermia and vasoconstriction of blood vessels , thus further reducing blood flow to the injury. Cover burn with plastic cling film lengthways along the burn (do not wrap circumferentially)
• Do not apply plastic cling film to face (use paraffin ointment)
• Do not apply plastic cling film to a chemical burn
➢ Appropriately consented photos of burns prior to dressings are useful for ongoing management
➢ Prevent hypothermia
o Remove wet clothes/dressings after initial cooling
o Cover the wound after assessment
o When possible, warm intravenous fluids and the room
Tap water is acceptable for flushing eyes exposed to chemicals. Tissue destruction may continue for up to 72 hour after contact with some chemicals.
EMERGENT PHASE :
The emergent ( resuscitative ) phase is the time required to resolve the immediate , life threatening problems resulting from burn injury. This phase usually last up to 48 hours from the time the burn occurred.
The primary concerns are the onset of hypovolemic shock and edema formation. The emergent phase ends when fluid mobilization and diuresis begins.
EMERGENT PHASE :
Hypovolemic shock caused by a massive shift of fluids out of the blood vessels as a result of increased capillary permeability and can begins as early as 20 minutes postburn. As the capillary walls become more permeable water , sodium , and plasma proteins ( especially albumin) move into their interstitial spaces and other surrounding tissue.
Fluid management:
Replacing fluids and electrolyte is an essential part of the treatment of burns victim and initiated as soon as possible as the severity of the burns and the patient condition is the unknown.
Fluid therapy is the started within an hour after a severe burn to prevent hypovolemic shock. Fluid administered during the 1st 48 hour are given to maintain circulating blood volume . The parkland formula was introduced in the 1970 and has been accepted worldwide for fluid resuscitation. The formula calculate the volume of fluid required based on TBSA involved
1) Parkland formula:
4ml × Body weight (kg) ×TBSA (%) = Total fluid volume in 1st 24 hours (1/2 of volume given in 1st 8 hours, ½ of the volume given over next 16 hour) Initial 24 hours : Ringer lactated ( RL) solution 4 ml / kg/% burn for children.
RL solution is added for maintenance of children:
• About 4ml/kg/hr for children weighing 0-10 kg
• About 40 ml /hr+ 2ml/hr for children weighing10-20 kg
• About 60 ml/ hr + 1 ml / kg/ hr for children weighing 20 kg or higher.
According to the formula no colloid should be administered in the initial 24 hours.
Next 24 hours :
Colloid are given as 20-60 % calculated plasma volume . NO crystalloids should be given . Glucose in water is added in amounts required to maintain a urinary output of 0.5-1 ml/hr/kg in adult and 1 ml/hr/kg in children.
Modified Parkland formula:
Initial 24 hours : RL 4 ml /kg /% burn (adult) and next 24 hours : colloid infusion of 5 % albumin 0.3 – 1 ml / kg / % burn / 16 / hr is started.
2) Consensus formula :
Lacted ringer solution ( or other balanced saline solution ):
2-4 mL Ringers Lactate x weight in kg x % TBSA= mLs in first 24 hours. Give half of this total in the first 8 hours post burn : Pediatrics use 3 mL: Electrical injuries use 4mL.
3. Evans formula
Normal saline at 1 ml/kg/% TBSA burn colloid at 1 ml/kg/% TBSA burn. For second 24 hours, give half of the first 24-hour requirements " D5W (dextrose 5% in water) 2000 ml.
4) Brooke army formula :
2mls x body surface areas burned (BSAB) x weight. The Parkland formula is 4mls x body surface areas burned (BSAB) x weight. Both formulas estimate the first 24 hour fluid requirements from the time of the burn, with half the amount given in the first 8 hours.
Assessment of adequacy of fluid resuscitation :
➢ Monitor urine output ( adult greater than 1ml/kg / hour)
➢ Daily weight
➢ Vital signs
➢ Heart rate and blood pressure
➢ CVP
➢ Level of consciousness
➢ Laboratory values
Antibiotic protocol in burns:
Patient care is improved by promoting the best practice in antibiotics prophylaxis and therapy Antibiotic will be given only when patient actually requires . If the the clinical condition is improving in general then antibiotics strategy should not changed. However if there is no clinical response within 72 hours the clinical diagnosis the choice of antibiotic and or possibly of a secondary infection should be reconsidered. The antibiotic should be given for the minimum length of time that is effective.
Antibiotic protocol in burns:
Commonly used topical agents include combination antimicrobial ointments, silver sulfadiazine, bismuth-impregnated petroleum gauze, mafenide, and chlorhexidine Other agents such as honey, povidone-iodine, and Dakin's solution are less commonly used. Combinations of antimicrobials with topical antifungal agents have also demonstrated some efficacy for the local treatment of burns
DRUGS
▪ Tetanus immunization
▪ Analgesic : Morphine , Fentanyl, methadone, NSAID (ketorolac) , Adjutant analgesics
▪ Sedatives: Midazolam, intrazepam,
▪ Antidepressant : Sertraline
▪ Anticoagulant : Heparin
▪ Nutritional support : vitamin A,C , E, and multivitamin minerals, zinc , iron
▪ Gastrointestinal support : Ranitidine , Nystatin .
SURGERY: -
Escharotomy
• The aim of the escharotomy is to release the pressure over the involved deeper tissues and to restore their circulation.
• Clinical indications for escharotomy include patient complaints of tingling or numbness in limbs.
• The incisions should extend from burnt skin to unburnt skin ideally, or at least into areas of more superficial burns, down to subcutaneous fat, and release any constrictions. In the limbs, incisions should be made in the midaxial line, both medially and laterally, and on the chest and abdominal wall, the incisions are made in the midaxillary lines, which can be joined by a transverse incision below the costal margin to allow adequate release.
• The wound edges should be adequately parted upon incision; any residual constrictions should be checked by running a finger along the length of the incision.
Fasciotomy:
• Fasciotomies are performed when there are circumferential burns.
• It is a surgical procedure to incise fascia to relieve pressure which otherwise would have resulted in loss of circulation to the tissue.
• It is a limb-saving method which is done to treat compartment syndrome.
Facial reconstructive surgery :
Reconstructive burn surgery is a procedure performed by a plastic surgeon after the initial wounds from a burn have healed . the goal of the surgery is to increase the function and restore the appearance of the skin . Some of these procedural involve several months of preparation to improve tissue .
NURSING MANAGEMENT
➢ Monitor hemodynamically status
➢ Keep accurate record of intake and output to monitor fluid loss and gain .
➢ Maintain IV solution containing electrolyte at consistent flow rate
➢ Monitor manifestations of electrolyte imbalance to detect early changes of electrolyte imbalance
➢ Provide optimal pain relief with prescribed analgesics to manage pain.
➢ Assure pre-treatment analgesia prior to painful procedures
➢ Maintain sterile dressing technique when performing wound care
➢ Monitor systematics and localized agent and symptoms for infection
ACUTE PHASE
Begins 48 to 72 hours after the burn injury. In this phase the extracellular fluid start mobilize and start diuresis. This phase complete when wound is covered by skin graft or wound are healed. This may take weeks or many months. Escher begins to separate fairly after injury . Re epithelialization begins at wound margin and appears as red/pink scar tissues The predominant therapeutic interventions in the acute phase are
1) Wound care
2) Excision and grafting
3) Pain management
4) Physical and occupational therapy
5) Nutritional therapy
1) WOUND CARE :
Goal : Prevent infection by cleansing and debriding the area of necrotic tissue that would promote bacterial growth and promote wound re-epithelialization and or successful skin grafting.
Wound care consist of ongoing observation , assessment , cleansing , debridement and dressing reapplication. Nonsurgical debridement , dressing changes topical antimicrobial therapy , graft care and donor site care are performed as often as necessary , depending on the topical cream or dressing ordered.
Enzymatic debriders made of natural ingredient , such as collagen , may ne used for enzymatic debridement of burns wounds, which speeds up the removal of dead tissue from the healthy wound bed.
Cleans wound with the soap and water or normal saline moistened gauze to the remove the old antimicrobial agent. During the debridement phase , cover the wound with topical antimicrobial creams( e.g. silver sulfadiazine) or silver impregnated dressing.
Dressings — A variety of antimicrobial agents can be applied to the burn wound surface, which is then covered with one of several dressing materials (eg, gauze, nonadherent films, honey , bactrigras dressing )
2) DEBRIDEMENT AND SKIN GRAFTING
• If patient is stable, then early excision is done within 48 hours.
• At a time, 15-20% dead skin is excised, and the wound is covered by autograft or allograft, and sometimes sandwich grafting is used.
• If patient's condition is not stable, then delayed debridement is done after 15-20 days, after patient becomes stable, followed by skin grafting.
• In the care of unavailability of autograft, for high percentage of burns , glycerol preserved allograft from cadaver is used as temporary biological dressing material
• Biologic grafts — Biologic graft materials that can be used for temporary coverage of burn wounds include allografts, xenografts, and others (eg, human amnion).
• Semibiologic skin substitutes are temporary biosynthetic dressings that are meant to reduce the number of dressing changes and facilitate healing. The semipermeable nature of these dressings allows wound exudate to be absorbed by the external bulky dressing.
• Biobrane is used to cover donor sites and aid in coverage of large surface area burns, including hands, feet, and joints
3) PAIN MANAGEMENT
Burn patient experience two kind of pain
1) Continuous background pain that might be present throughout the day and night
2) Treatment induced pain associated with dressing , changes , ambulation and rehabilitation activities.
• With background pain a continuous iv infusion of an opioids(e.g. hydromorphone) allows for a steady , therapeutic level of medication.
• Anxiolytics which can potential analgesic are also can indicated and include lorazepam and midazolam.
• Adjuvant analgesic such as gabapentin and pregabalin also potentiate opioids.
• Fentanyl also used.
• Some pain can be manged using nondrug strategies . mind body intervention such as relaxation breathing, guided imagery, hypnosis, biofeedback, and musical therapy .
• Patient control analgesia is used in selected circumstances in some burn centers
4) PHYSICAL AND OCCUPATIONAL THERAPY:
Continuous physical therapy ,passive and active ROM should be performed on all joints. Ensure that the patient with neck burns continue to sleep without pillows or head hanging slightly over the top of the mattress to encourage hyper-extension. Maintain the occupational therapy schedule for wearing custom fitted splint , which are designated to keep joint in functional positions.
5) NUTRITIONAL THERAPY
When the wounds are still open the burn patient is in a hypermetabolic and highly catabolic state. Encourage patient to eat high protein, high carbohydrate foods to meet caloric needs.
• A burns patient's nourishment depends upon early oral feeding.
• It should be started within 48-72 hours just after completion of resuscitation. Burn patients find difficulty while chewing the food so special diet has to be prepared for them and administered through nasogastric tube.
• Small measured quantity is given per hourly basis and monitored continuously.
• The buttermilk diet is the safe and well-tolerated food for the burns patients, it contains 1 kcal energy per mL. It consists of curd-1 L, eggs-four, banana-four, sugar-four tablespoons.
• The total volume to be made is 1,760 mL, energy content is 1,760 kcal, protein content is 60 g, and carbohydrate content is 340 g. The starting quantity is 10 mL/h for every 6 hours to reach a maximum of 3-5 mL/kg/h for children and 2 ml/kg/h for adults.
NURSING MANAGEMENT
➢ Weight patient daily and monitor trends to detect early signs of fluid imbalance.
➢ Teach the use of non pharmacological technique before and after and if possible during painful activity .
➢ Monitor patient satisfaction with the pain management at specified interval
➢ Apply an appropriate burn cream and or dressing to the skin to promote healing.
➢ Compare and record regularly any changes to the wound to promote healing .
➢ Provide physical isolation measures to prevent infection .
➢ Provide patient with high protein , high calorie , nutritious finger food and drink that can be readily consumed to meet nutritional needs .
➢ Monitor food/ fluids ingested and calculate daily caloric intake to assess adequacy of diet.
REHABILITATION PHASE :
The formal rehabilitative phase begin with the patient wounds have healed and he or she engaging in some level of self care. This may happen as early as 2 weeks or as long as 7 to 8 month after burn injury.
Goal: 1) work toward resuming a functional role in society
3) Rehabilitate from any functional and cosmetic postburn reconstructive surgery that may be necessary.
➢ Focus on is upon wound healing , psychosocial support , self image, lifestyle and restoring maximal functional abilities so the patient can have best quality life both personally and socially.
➢ Vocational counselling and support groups may assist the patient.
➢ Reconstructive surgeries for improving body appearance and function.
EMOTIONAL / PSYCHOLOGICAL NEEDS OF PATIENT AND CAREGIVERS :
To manage the enormous range of emotional responses that the burn patient may exhibit , assess the circumstances of the burn ( e.g. cause , people involved) , family relationship and previous coping experiences with stressful stimuli.
At any time the patient may experience a variety of emotion such as fear , anxiety , anger , guilt, and depression.
Burn survivors frequently experience thoughts and feeling that are frightening and disturbing , such as guilt about the burn incident , relieving of the frightening burn experience , fear of dying , concern about future therapy and surgery frustration with ongoing discomfort and treatment and hopelessness about the future.
NURSING MANAGEMENT :
➢ Determine the impact of the pain experience on quality of life (e.g. sleep, appetite, activity , cognition, mood , relationship of job, and role responsibility) to plan long term pain management
➢ Assist patient and family to seek and obtain support to manage residual pain .
➢ Monitor appropriateness of diet order to meet daily nutritional needs to promote excess weight gain.
➢ Refer for diet teaching and planning to meet long term nutritional needs.
NURSING DIAGNOSIS :
• Acute pain related to destruction of skin/ tissue as evidence by restlessness.
• Impaired skin integrity related to distruption of skin surface with destruction of skin layers as evidence by absence of viable tissue.
• Ineffective tissue perfusion related to interruption of arterial/ venous blood flow as evidence by oedema.
• Impaired physical mobility related to neuromuscular impairment as evidence by inability to do activity.
• Disturbed body image related to situational crisis of traumatic events as evidence by negative feeling about body.
•Imbalance nutrition less than body requirements related to hypermetabolic state as evidence by anorexia.
GENERAL NURSING MANAGEMENT:
The nursing assessment focuses on the major priorities for any trauma patient; the burn wound is a secondary consideration.
✓ Obtain history. Assess body temperature, body weight, history of preburn weight, allergies, tetanus immunization, past medical surgical problems, current illnesses, and use of medications.
✓ Arrange for patients with facial burns to be assessed for corneal injury.
✓ Continue to assess the extent of the burn; assess depth of wound, and identify areas of full and partial thickness injury.
✓ Assess neurologic status: consciousness, psychological status, pain and anxiety levels, and behaviour.
✓ Assess patient’s and family’ s understanding of injury and treatment. Assess patient’s support system and coping skills.
✓ Focus on the major priorities of any trauma patient. the burn wound is a secondary consideration, although aseptic management of the burn wounds and invasive lines continues.
✓ Assess circumstances surrounding the injury. Time of injury, mechanism of burn, whether the burn occurred in a closed space, the possibility of inhalation of noxious chemicals, and any related trauma.
✓ Monitor vital signs frequently. Monitor respiratory status closely; and evaluate apical, carotid, and femoral pulses particularly in areas of circumferential burn injury to an extremity.
✓ Start cardiac monitoring if indicated. If patient has history of cardiac or respiratory problems, electrical injury.
✓ Check peripheral pulses on burned extremities hourly; use Doppler as needed.
✓ Monitor fluid intake (IV fluids) and output (urinary catheter) and measure hourly. Note amount of urine obtained when catheter is inserted (indicates preburn renal function and fluid status).